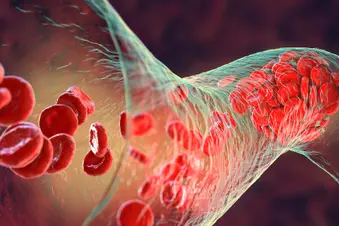
Atypical hemolytic uremic syndrome (aHUS) causes tiny blood clots to form in your blood vessels. Because of these clots, blood can’t flow the way it should to your organs. Doctors typically consider aHUS a disease that primarily affects your kidneys, but blood clots can cause serious damage in other organs such as your brain, gastrointestinal tract, liver, lungs, and heart.
This form of the disease isn’t the same as typical hemolytic uremic syndrome, which is caused by toxins made by E. coli. Typical hemolytic uremic syndrome is much more common than aHUS.
There are three common features in people with aHUS:
Hemolytic anemia. This is the destruction and breakdown of red blood cells. Your body struggles to make new red blood cells to replace the ones that have broken down, and you get anemia (pale skin, shortness of breath, feeling cold and tired).
Thrombocytopenia. This condition causes easy bruising and bleeding. You get it when you have fewer platelets in your blood than normal. Platelets are cells that help form a blood clot to stop bleeding. When you have aHUS, many of your platelets are being used to form abnormal blood clots.
Kidney failure. The abnormal blood clots that form in aHUS keep your kidneys from filtering waste and fluids the way they’re meant to, which can lead to end-stage renal disease (kidney failure).
There is no cure for aHUS. But you can treat it with medicines and therapies that boost your red blood cell and platelet production, help protect your kidneys, and occasionally exchange some of your blood with healthy blood.
Who Gets aHUS?
Only about 1 in 500,000 people in the U.S. get aHUS each year. This makes it an extremely rare disease. You’re 10 times more likely to get typical hemolytic uremic syndrome than aHUS.
In kids with aHUS, an equal number of boys and girls have it. In adults, more women have it than men. Researchers think this may be because one of the triggers to developing the disease is pregnancy.
About half of all cases of aHUS happen because of a genetic mutation. Some people who get the disease this way inherit the mutation from a relative, which is why you’re more likely to have aHUS if you have a parent, grandparent, or sibling who has it. But sometimes the genetic mutation happens randomly. However, a diagnosis of aHUS doesn’t require the identification of a mutation.
Symptom Triggers
Even if you have the genetic mutation that causes aHUS, often it takes another event, or trigger, for the disease course to start in your body.
Certain health conditions can set off aHUS, including:
- Pregnancy
- Cancer
- Infection
- Organ transplantation
Taking certain medications can be the trigger. These include:
- Certain chemotherapies for cancer
- Medications that suppress (dampen) your immune system
- Blood thinners
- Birth control pills
- Anti-inflammatory medications
Living With aHUS
You’ll have aHUS your whole life. While you can’t prevent it, you can take steps to be sure you’re managing your condition well. Your quality of life and disease outcome depend on several factors, including:
- How old you are when you’re diagnosed
- How well your aHUS responds to treatment
- Your overall health
Ask your doctor to help you better understand how to avoid symptom episodes. Be on the watch for signs you’re flaring, including:
- Feeling like you’re out of energy (fatigue)
- Pale skin
- Nausea or vomiting
- Peeing less
- Blood in your pee
- High blood pressure
- Shortness of breath
- Swelling
- Fever
Take note if you feel generally unwell, like if you have low-level sickness you can’t shake. In some cases, you may have brain and nerve symptoms such as confusion, but this is rare.
See a doctor right away if you’re dealing with:
- Peeing very little
- Confusion or altered mental state
- Severe swelling
- Trouble breathing
Questions for Your Doctor
As you learn more about your condition and how to best live with it, ask your doctor questions about your specific disease course and symptoms. You might want to ask:
- How is my overall condition with aHUS?
- What triggered my symptoms?
- What are some ways I can prevent flares in the future?
- Which symptoms should I look out for?
- How often should I check in with you to manage my disease?
Show Sources
(Photo Credit: iStock/Getty Images)
SOURCES:
American Kidney Fund: “aHUS (atypical hemolytic uremic syndrome).”
MedlinePlus: “Atypical hemolytic-uremic syndrome.”
NORD: “Atypical Hemolytic Uremic Syndrome.”
Cleveland Clinic: “Atypical Hemolytic Uremic Syndrome.”