Questions to Ask Your Doctor About EGFR-Positive NSCLC

What Is EGFR-Positive NSCLC?
EGFR is shorthand for epidermal growth factor receptor. It’s a protein that tells cells when to grow and divide. When there’s a mutation, or change, in its DNA, the messages it sends your cells change. This can lead to the growth of cells that cause cancer. In the U.S., about 85% of all lung cancers are non-small-cell lung cancers (NSCLCs), and roughly 15% of all lung cancers have an EGFR-positive mutation.
Which EGFR Mutation Do I Have?
There are more than 70 EGFR mutations. Many are either additions (“insertions”) to or subtractions (“deletions”) from the EGFR DNA genetic code. It’s critical for your treatment that your medical team first pinpoints your specific mutation. Certain rare mutations don’t respond to the drugs given for the more common ones.

When Will You Do a Biomarker Test?
Biomarker tests show what kind of EGFR mutation you have. You might have already had a biomarker test on a tissue sample, or biopsy, from your lung. This is the main way to find out the genetic makeup of your tumor. Your doctor may also do a test called a blood or liquid biopsy on a blood sample. A liquid biopsy technique called NGS, or next-generation sequencing, can test for several biomarkers at once with a small sample.

What Is the Stage of My Cancer?
The stage of your EGFR-positive NSCLC is another important clue to help guide your treatment. Stages range from occult (or hidden) to 0 to IV, with many sub-stages. Treatments vary by stage and even by sub-stage.

What Are My Treatment Options?
The stage of your cancer will guide your treatment. If possible, treatment starts with surgery to remove the tumor. You may take targeted medications called EGFR inhibitors that block the faulty signals that tell cancer cells to grow. These may be tyrosine kinase inhibitors (TKIs) that you take by mouth or monoclonal antibodies that you get as an IV. Chemotherapy, radiation, and immunotherapy are also options.

What Are the Goals of My Treatment?
In early stages, surgery may be able to cure the cancer. In late stages, the goal is to slow its growth to extend survival time from months to years. The time frame is longer for the most common mutations but shorter for rarer ones. In the latest stages, your treatment will focus on keeping you comfortable and giving you the best possible quality of life.

What Treatments Are on the Horizon?
Researchers are constantly looking for treatments that work better for all mutations, including better versions of EGFR inhibitors like TKIs. One possibility is a combination therapy that pairs immunotherapy with chemotherapy.

What Are the Side Effects of EGFR Inhibitors?
Ask about the common side effects of EGFR inhibitors so you can be better prepared. They include skin reactions like a pimply rash, dry skin, itchiness, or changes to hair and nails. This is because these drugs also change the way skin cells function. Many people get diarrhea, which can lead to dehydration and weakness if severe. Mouth sores and loss of appetite are also possible.
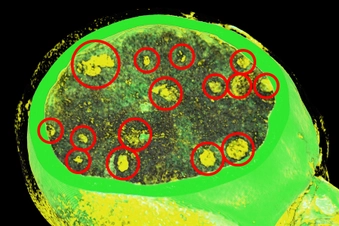
How Do I Know if My Cancer Has Spread?
It’s very common for EGFR lung cancer to spread, or metastasize, to the brain. Ask about symptoms you might have and tests to look for signs of these brain metastases. Because some of the drugs that target EGFR can cross the blood-brain barrier, they can treat lung cancer that has spread to the brain. Some brain metastases are treated directly with radiation.

Should I Join a Clinical Trial?
Depending on your specific type of EGFR-positive NSCLC, you might be a candidate for one of the many clinical trials for new lung cancer treatments. People in a clinical trial usually get either the standard treatment or the new treatment under investigation. Ask your doctor about trials that you may qualify for.

What if My Cancer Comes Back?
EGFR inhibitors can often control lung cancer for several months or even years. But cancer cells are always changing. They often become resistant to cancer drugs. This is called acquired resistance. If this happens, ask if your doctor could repeat a biomarker test to look for a new mutation that might respond to another drug. Some people with lung cancer that progresses benefit from platinum-based chemotherapy.
Show Sources
IMAGES PROVIDED BY:
1) iStock/Getty Images
2) Moment/Getty Images
3) Image Source/Getty Images
4) Science Photo Library/Getty Images
5) iStock/Getty Images
6) E+/Getty Images
7) (Left to right) iStock/Getty Images, STEVE GSCHMEISSNER/Science Source
8) DR P. MARAZZI/Science Source
9) VSEVOLOD ZVIRYK/Science Source
10) Cultura RF/Andrew Brookes/Medical Images
11) iStock/Getty Images
SOURCES:
EGFR Lung Cancer Resisters.org: “Epidermal growth factor receptor.”
Lung Cancer Foundation of America: “What is EGFR-positive lung cancer and how is it treated?” “Lung Cancer Facts: 29 Statistics and Figures.”
MD Anderson: “MD Anderson EGFR Classification licensed by BostonGene and Tempus to provide new insight on atypical mutations in lung cancer.”
American Lung Association: “EGFR and Lung Cancer,” “EGFR Exon 20 Insertion Mutation and Lung Cancer,” “EGFR Exon 20 Lung Cancer,” “Your Lung Cancer, Your Goals.”
Biology: “Next Generation Sequencing Technology in Lung Cancer Diagnosis.”
National Cancer Institute: “Non-Small Cell Lung Cancer Treatment (PDQ) – Patient Version.”
ASCO Daily News: “ASCO Annual Meeting 2023: Improving Outcomes in Glioma, Hodgkin Lymphoma, Lung Cancer, Ovarian Cancer, and Rectal Cancer,” “Recent Developments in Targeting EGFR Exon 20 Mutations in Non-Small Cell Lung Cancer.”
American Cancer Society: “Treatment Choices for Non-Small Cell Lung Cancer, by Stage,” “Targeted Drug Therapy for Non-Small Cell Lung Cancer.”
Onco Targets and Therapy: “Amivantamab in the Treatment of Metastatic NSCLC: Patient Selection and Special Considerations.”
The Lancet: “Overall survival in advanced epidermal growth factor receptor mutated non-small cell lung cancer using different tyrosine kinase inhibitors in The Netherlands: a retrospective, nationwide registry study.”
Cancer Cell: “Poziotinib for EGFR exon 20 mutant NSCLC: clinical efficacy, resistance mechanisms and impact of insertion location on drug sensitivity.”
Current Oncology: “Managing treatment-related adverse events associated with EGFR tyrosine kinase inhibitors in advanced non-small-cell lung cancer.”
Therapeutic Advances in Medical Oncology: “Management of diarrhea induced by EGFR-TKIs in advanced lung adenocarcinoma.”
Lung Cancer: “Treatment strategies and outcomes for patients with EGFR-mutant non-small cell lung cancer resistant to EGFR tyrosine kinase inhibitors: Focus on novel therapies.”
Frontiers in Immunology: “Immunotherapy for EGFR-mutant advanced non-small-cell lung cancer: Current status, possible mechanisms and application prospects.”