- Overview
- Symptoms
- Risks, Prevention & Screening
- Tests & Diagnosis
- Types
- Your Breast Cancer Care Team
- Treatment
- Living With Breast Cancer
- Remission & Recurrence
- Advanced Breast Cancer
- Support & Resources
- Appointment Prep
- View Full Guide
Breast Cancer Treatment and Recovery Timeline: What to Expect from Start to Finish



Detect Your Breast Cancer (1-3 weeks)
You might first notice a lump or other breast changes during a routine self exam and report it to your doctor. Or a mammogram screening might spot a tumor – a mass of abnormal tissue – sooner than you can feel it yourself. Your doctor will schedule a diagnostic mammogram, which is a more detailed X-ray. Sometimes they’ll order more imaging, such as an ultrasound of your breast.

Get Your Diagnosis (1-2 weeks)
Your diagnostic test results likely will be ready while you’re at your follow-up appointment. You’ll get a letter, too. Your doctor might order an MRI if you have dense breast tissue or other imaging results aren’t clear. If the tests show that the mass is solid, your radiologist may recommend a biopsy, in which small bits of breast tissue are removed and examined under a microscope.

Get Your Pathology Report (1-2 weeks)
A pathologist – a doctor trained in making diagnoses – will study the tissue samples taken during your biopsy. They’ll make a report of their findings and share them with your doctors. It’ll show whether your breasts have cancer cells. Your pathology report might be ready in two or three days, but sometimes it can take a week or longer.

Get a Second Opinion (Right After Diagnosis)
If you’ve gotten a breast cancer diagnosis, you likely still have time to ask another specialist or medical team for a second opinion, if you wish. They might:
- Confirm your first doctor’s diagnosis and plan
- Give more details about the type and stage of your breast cancer
- Suggest additional treatment options you hadn’t considered
- Recommend a different course of action

Schedule Your Surgery (3-8 weeks)
Most types of breast cancer require surgery to remove it. You might have a lumpectomy, which removes part of your breast, or a mastectomy, which removes the entire breast. Most research agrees it's best to schedule surgery before eight weeks after diagnosis (56 days or less).

Recover From Surgery (4-6 weeks)
Your upper body might feel sore for a few weeks after surgery. You’ll be offered painkillers and given daily exercises to loosen up your arms and shoulders. You might have fatigue. You'll likely get your stamina back and return to normal activities after about a month.

If You Need Radiation Therapy (3 to 8 weeks after surgery)
Your doctor might recommend radiation therapy to cut down the risk of breast cancer returning after you have surgery. If you’re having chemo, radiation therapy usually starts three to four weeks after chemo treatments end. However, radiation therapy can be used at any stage of breast cancer treatment.

If You Need Chemotherapy (4-8 weeks after surgery)
Chemotherapy is often combined with other breast cancer treatments. You might receive it after surgery to get rid of remaining cancer cells and cut down the risk of the cancer coming back. Sometimes chemo is used to reduce larger cancers before surgery.
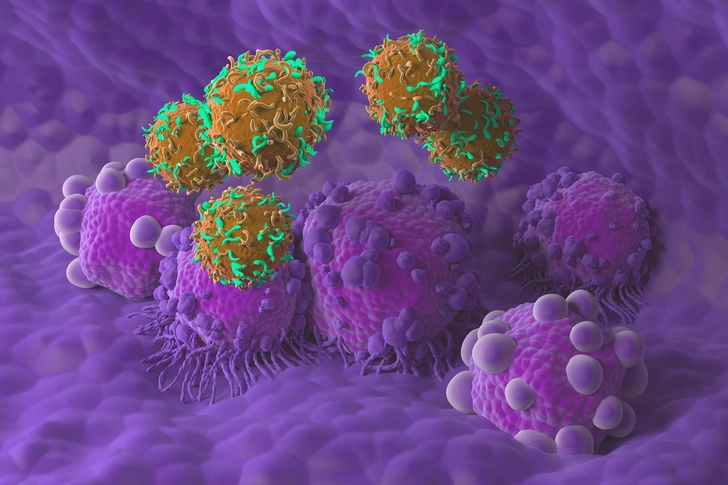
Targeted Therapies (used with chemotherapy)
Targeted therapy uses meds to kill or halt growth of certain proteins on breast cancer cells. It’s usually used in combo with chemotherapy to treat metastatic, or later-stage, breast cancer.

Hormone Therapy (months to years)
Hormone therapy is a common treatment after surgery to help cut the risk of the cancer returning. Sometimes it’s given before surgery. Hormone therapy usually continues for at least five years.

Get Rehabilitation Care (ongoing)
Rehabilitation care offers support all along the breast cancer treatment timeline: during breast cancer treatment, as you’re recovering, and into remission and beyond. The rehabilitation care team can ID and help manage pain, address side effects from treatment, treat mental fog that’s common after treatment, and much more.

Keep Up a Healthy Lifestyle (ongoing)
The lifestyle choices that have always kept you healthiest will also boost your well-being post-treatment. Living well also will lessen the risk of the cancer returning. The usual healthy habits apply: eat a well-balanced diet, aim to stay at the right weight for your body size and type, be active, and find wholesome ways to manage stress.

Follow Through on Checkups (as scheduled)
After you finish treatment, it’s key to go to all of your follow-up appointments and stay on top of prescribed protocols such as regular mammograms. (If you have hormone treatment, you’ll need regular pelvic exams and bone density tests.) If symptoms return, your doctor will want to run diagnostic and imaging tests and maybe do a biopsy.

Plan Long-Term Recovery (years beyond treatment)
Ask your doctor to compile a survivorship care plan for you. This will include:
- A summary of your breast cancer diagnosis, all testing done, and treatments you had
- A list of possible long-term side effects and what to do about them
- Lifestyle suggestions with specifics about diet and exercise
- A schedule of follow-up appointments and exams and screenings

Remember, Everyone’s Different
Everyone’s journey is not the same. Life going forward can mean being in remission, having longer-term treatments, or living with later-stage breast cancer. You might go through body changes, have later side effects, or still feel emotions from your experience or different aspects of treatment. But you can look forward to new treatments and approaches that continually improve and offer even greater hope.
IMAGES PROVIDED BY:
- iStock/Getty Images
- iStock/Getty Images
- iStock/Getty Images
- Moment/Getty Images
- WebMD
- Moment/Getty Images
- Mark Kostich/Getty Images
- SeventyFour/Getty Images
- Science Photo Library/Getty Images
- Moment/Getty Images
- DigitalVision/Getty Images
- Moment/Getty Images
- Corbis/Getty Images
- E+/Getty Images
- Moment/Getty Images
SOURCES:
National Breast Cancer Foundation: “Breast Self-Exam,” “Diagnostic Mammogram.”
American Cancer Society: “Getting Called Back After a Mammogram,” “After a Breast Cancer Diagnosis,” “Your Breast Pathology Report: Breast Cancer,” “Hormone Therapy for Breast Cancer,” “Targeted Drug Therapy for Breast Cancer,” “Follow-up Care After Breast Cancer Treatment.”
Penn Medicine: “Breast Biopsy.”
Breastcancer.org: “Getting a Second Opinion.”
JAMA Surgery: “Reexamining Time From Breast Cancer Diagnosis to Primary Breast Surgery.”
Cleveland Clinic: “Breast Cancer Surgery.”
Mayo Clinic: “Radiation Therapy for Breast Cancer,” “Chemotherapy for Breast Cancer,” “After Breast Cancer Treatment: How to Adapt Your Lifestyle for Optimal Health.”
Annals of Surgery Oncology: “Timing and Delays in Breast Cancer Evaluation and Treatment.”
Michigan Medicine: “5 Reasons Rehabilitation Care is Important After Breast Cancer.”
Breast Cancer Research Foundation: “What We Talk About When We Talk About Breast Cancer Survivorship.”