Keytruda (pembrolizumab) and Keytruda Qlex (pembrolizumab/berahyaluronidase alfa) are a type of cancer treatment called immunotherapy. Immunotherapy works by using the body's immune system to fight cancer cells. Keytruda is designed to help the immune system fight a type of kidney cancer called renal cell carcinoma (RCC). Below you’ll find common questions and answers about Keytruda to help decide whether it’s right for you.
How Does Keytruda Work for RCC?
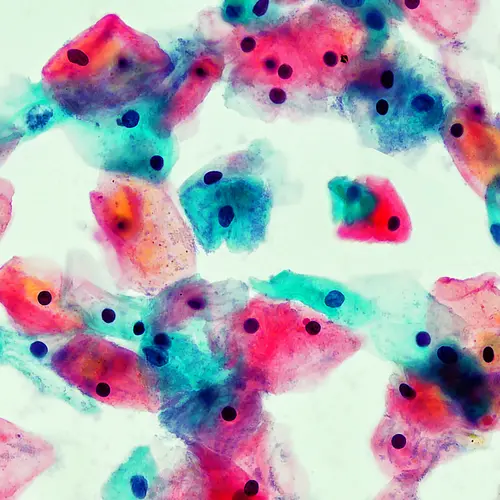
Some cancer cells have what are called checkpoint proteins known as PD-L1 on their cell surface. Some immune cells in our bodies called T cells have proteins on their surface that bind to PD-L1. When these proteins bind to each other, the T cells in our body get turned “off,” which stops them from killing cancer cells. Keytruda acts on proteins on the T cell and prevents these proteins from binding to PD-L1 proteins on the tumor cell. This turns the T cell back “on” and allows it to do its job of attacking and killing the tumor cell.
What Kinds of RCC Does Keytruda Treat?
- RCC that has spread or cannot be removed by surgery (advanced)
- RCC that it is at risk of coming back (recurring) after surgery
How Will I Get Keytruda?
Both Keytruda and Keytruda Qlex contain pembrolizumab, but Keytruda is given as an IV infusion over 30 minutes while Keytruda Qlex is given as an injection under the skin (subcutaneous) over 1 minute. Both products are given by a health care professional. Doses are usually given every three or six weeks. Your health care provider will decide the dose and schedule that is right for you. They may pause or stop your treatment if your cancer gets worse (progresses) or if you have certain side effects.
How Was Keytruda Studied for RCC?
Keytruda was studied in people with advanced RCC who had not gotten any prior treatment for their cancer. People in this study got either Keytruda plus an oral medicine called axitinib, or another oral chemotherapy medicine used to treat RCC, called sunitinib. This trial looked at overall survival (OS) and progression free survival (PFS), which measured how long people lived without their disease progressing. It also looked at objective response rate (ORR), which measures the percentage of people who had either a complete or partial response to treatment. There were 861 people in this trial. The median age was 62, with a range of 26 to 90, and 38% were 65 or older. Most people were male (73%). Seventy-nine percent of people were White and 16% were Asian. People in this trial were followed for an average of 43 months. At that time, the median OS was 45.7 months in the Keytruda group, versus 40.1 months in the sunitinib group. The PFS was also longer in the Keytruda group, at 15.7 months, versus 11 months in the sunitinib group. This means that half of the people in the Keytruda group lived at least 15.7 months without their disease progressing and lived at least 45.7 months overall. Likewise, the ORR was 60% in the Keytruda group and 40% in the sunitinib group.
Keytruda was also studied in people with RCC along with another oral medicine called lenvatinib. People in this trial got either Keytruda plus lenvatinib, lenvatinib plus everolimus, or sunitinib. There were 1,069 people in this study, and they were evenly divided among the three groups. The median age was 62 years, with a range of 29 to 88 years. Forty-two percent were 65 or older, and 75% were male. Seventy-four percent of people were White, 21% were Asian, 1% were Black, and 2% were other races. This trial looked at PFS and objective response rate (ORR). The median PFS was longer in the Keytruda group, at 23.9 months, versus the sunitinib group, at 9.2 months. The ORR was also longer in the Keytruda group, with 71% of people having a response, as opposed to 36% in the sunitinib group.
A study was also done in people who had high-risk RCC after they had surgery to remove their cancer (nephrectomy). In this study, people got either Keytruda or a placebo. This study looked at disease-free survival (DFS), which looked at how long people lived without the cancer recurring or growing to other parts of the body (metastasizing). It also looked at the OS. There were 994 people in this trial, and about half were in each group. The median age was 60 years old, with a range of 25 to 84, and 33% were 65 or older. Seventy-one percent of the people were male. Seventy-five percent of the people in this study were White, 14% were Asian, 1% were Black or African American, 1% were American Indian or Alaska Native, 1% were multiracial, 13% were Hispanic or Latino, and 7% were of unknown race. At 24 months, there was 32% reduction in the risk of recurrence. DFS for the Keytruda group was 77%, and DFS for the placebo group was 68%. OS was also better in the Keytruda group, and the study showed a 38% reduction of the risk of death in those people.
How was Keytruda Qlex studied for RCC?
Keytruda Qlex contains the same medicine as Keytruda, but it is given as an injection under the skin (subcutaneous), while Keytruda is given as an intravenous infusion. The studies described above for Keytruda were also used to show that Keytruda Qlex is effective for treating RCC.
Another study was done with Keytruda Qlex to see if there was any difference in blood levels when the medicine was given under the skin as compared to giving it by intravenous infusion. This study found comparable blood levels between Keytruda Qlex and Keytruda. The safety of Keytruda Qlex was also generally similar to Keytruda.
What Are Some Unique Considerations to Be Aware Of?
Keytruda can harm a fetus. Your health care provider will discuss options for contraception while you take Keytruda. You should use an effective method of birth control while you are receiving Keytruda and for four months after your last dose. If you and your partner are pregnant or are planning to become pregnant, talk with your health care provider about your options. Keytruda may pass into your breast milk if you are breastfeeding. You should not breastfeed while you are getting Keytruda and for four months after your last dose.
Keytruda can cause very serious side effects. These include problems in your lungs, intestines, liver, hormone glands, kidneys, and skin. Problems can also happen in other organs and tissues. It is important to tell your health care provider as soon as you have any side effects, including chest pain, a fast heartbeat, shortness of breath, confusion, double or blurry vision, severe muscle pains, or bruising more easily than usual.
What Are the Side Effects of Keytruda, and How Can I Prevent or Manage Them?
Keytruda can cause severe side effects, including fatigue, skin reactions, diarrhea, and muscle or bone pain.
Feeling tired is a common side effect of Keytruda, but there are some things you can do to help increase your energy. Exercising each day, even if it is just for a short time, can help boost your energy. Eating a healthy diet of fruits, vegetables, lean protein, and whole grains while avoiding sugary foods may also help you fight fatigue. Your doctor may be able to give you medicines to treat other side effects such as depression, pain, or low blood counts, which may help with your fatigue.
Contact your health care provider right away if you notice any new rash or an existing rash that is getting worse; reddening of the skin; fever; blistering of the lips, eyes, or mouth; blisters on the skin; skin peeling; or dry skin. They will decide whether you should stop taking Keytruda. They may also recommend creams or antihistamines to help with your rash and itchiness. Skin reactions are a common side effect of Keytruda and can happen at any time after you start taking it and even after you stop. You may also be given a corticosteroid to treat your rash.
Let your health care provider know as soon as diarrhea starts, and start taking your diarrhea medicine. Drink more fluids to avoid losing too much of your body water (dehydration). Mild to moderate diarrhea can happen any time after you start taking Keytruda. Your health care provider may treat you with corticosteroids if your diarrhea is mild or moderate. If you have severe diarrhea, you may receive another immunosuppressive treatment given to you as an IV infusion.
You may also have muscle, bone, or joint pain while taking Keytruda. Your health care provider may recommend that you use over-the-counter pain relievers such as ibuprofen or Tylenol. You should contact your health care provider if you have pain that does not go away with over-the-counter medicines.
Keytruda, when used along with axitinib or lenvatinib, may cause oral toxicity, such as stomatitis (inflammation of the mouth). Good dental hygiene, such as brushing your teeth several times a day with a soft toothbrush and flossing at least once a day, can help prevent mouth sores and dry mouth. If you get mouth sores, you can use a mixture of baking soda, salt, and warm water to rinse your mouth. Avoiding spicy, acidic, and hard foods such as chips, and eating softer foods instead can help if you have mouth pain. You can try over-the-counter medications that help to numb your mouth sores, or your doctor may give you something to treat your pain if it becomes severe.
If you’re receiving Keytruda along with axitinib or lenvatinib, your health care provider may recommend taking certain medications to help prevent common side effects like nausea and vomiting. It’s important to follow their instructions carefully. Along with taking prescribed medications, you can ask your health care provider for more ways to manage or prevent side effects. For example, eating bland foods and having several small meals throughout the day, avoiding greasy foods, and drinking only small amounts of clear liquids can help manage nausea and vomiting.
If you have certain side effects while you take Keytruda, your health care provider may need to change how often you get infusions, pause your infusions, or even stop your medicine altogether. This will depend on how severe the side effect is and what type of treatment it requires.
These are not all the side effects you may have with Keytruda. Talk with your health care provider if you have side effects that bother you. In the U.S., you can report side effects to the FDA at www.fda.gov/medwatch or by calling 800-FDA-1088 (800-332-1088). In Canada, you can report side effects to Health Canada at www.health.gc.ca/medeffect or by calling 866-234-2345.
How Do I Know if Keytruda Is Working?
Your health care provider will regularly check how well Keytruda is working for your cancer by looking at results of tests such as blood tests and CT scans or MRI scans. You may notice improvements within a few weeks to months after starting Keytruda. The complete therapeutic effect can take longer, depending on individual factors and disease progression.
How Long Does Keytruda Stay in My System?
Keytruda remains in the body for several months after the last dose. Even after stopping Keytruda, immune-related side effects may continue. Regular follow-up is essential to manage any lingering side effects and ensure a smooth transition off the treatment.
How Can I Get Keytruda?
Your cancer doctor (oncologist) will arrange for you to receive Keytruda in a health care setting, such as a hospital or infusion center.
If you need support paying for Keytruda, the drugmaker may be able to help you. Check out their Merck financial support website at www.keytruda.com/financial-support/ to learn more about their patient assistance program or to ask your questions about insurance coverage and out-of-pocket costs. You can also contact the drugmaker at 855-398-7832.