What Is Endocarditis?
Endocarditis is a serious inflammation caused by an infection in the lining of your heart's chambers and valves. It happens when germs or bacteria from other parts of your body, such as your mouth, spread through your blood and attach to this lining. If the infection isn't treated with antibiotics or surgery, it can do permanent damage and can even be deadly.
The bacteria produces growths that appear on your heart valves, releasing enzymes and toxins that attack your heart tissue and produce holes in your valves, which can leak the harmful substances from your blood vessels and heart.
Endocarditis vs. myocarditis
Endocarditis and myocarditis are both types of heart inflammation. The difference lies in where the inflammation happens. The myocardium is the heart's middle layer, the muscular part. Myocarditis affects this layer, which produces the heart's contractions and release as it pumps blood. The endocardium, where endocarditis happens, is the inner layer of the heart. Myocarditis usually stems from a viral infection, such as a cold or the flu, and can eventually weaken the heart, while endocarditis is a bacterial or fungal infection.
Types of Endocarditis
There are several types of endocarditis:
Acute endocarditis. Acute infective endocarditis comes on suddenly and may quickly become life threatening if left untreated. It happens when an otherwise healthy heart valve is invaded by an aggressive germ such as staphylococcus, a common bacteria that lives on the skin, which can travel through the bloodstream into the heart. Once inside the heart, the bacteria begins to multiply, breaks off, and then reenters the bloodstream, moving into other parts of the body.
Subacute endocarditis. Also called chronic infective endocarditis, the subacute type develops more slowly — over a span of weeks or months. Subacute endocarditis is typically caused by groups of bacteria that live in the mouth and throat or the intestines of people with conditions such as colon cancer or diverticulitis. Usually, people with this form of endocarditis already have heart valves that are damaged. Vague symptoms can make subacute endocarditis hard to diagnose.
Prosthetic valvular infective endocarditis (PVE). This type of endocarditis develops after you've had a heart valve replacement. It happens when bacteria attaches to a replacement valve in the days, weeks, or months after surgery. It's important to watch for signs of PVE after your surgery and treat it as a medical emergency if you do notice symptoms, as early treatment can help prevent serious complications. PVE accounts for one-fifth of all endocarditis cases.
Nonbacterial endocarditis. This rare condition is caused by noninfected lesions (holes) in the heart valves and is commonly associated with a cancer diagnosis. It is usually found in an autopsy after someone's death. While doctors are unsure of its exact cause, they do know that the growths found in nonbacterial endocarditis are very different from those caused by a bacterial infection.
Endocarditis Symptoms
If you develop endocarditis, you may get sudden symptoms, or you may develop them over time. The way you feel will depend on how healthy your heart is and what caused your infection. The symptoms can also vary from person to person but may include:
Flu-like symptoms. You may develop a fever, chills, and night sweats. You might also feel achy in your muscles and joints.
Nausea. You could lose interest in food, feel sick to your stomach, or vomit.
Blood in your urine. You might be able to see it on your own, or your doctor might see it under a microscope.
Endocarditis heart murmur. Endocarditis can cause a new or additional heart murmur, which is an unusual, whooshing sound in your heartbeat, or changes to an existing one.
Endocarditis skin symptoms. These include tiny, painless bumps or spots may come and go on the palms of your hands or soles of your feet (Janeway lesions); small dark spots on your skin, in the whites of your eyes, or the roof of your mouth due to broken blood vessels; and painful, red bumps on your finger and toe pads called Osler nodes. Your skin also could be pale.
Endocarditis pain. You may have pain or tenderness on your left side under the rib cage. This may be a sign your spleen is trying to fight the infection.
Swelling and endocarditis. Endocarditis can cause swelling of your abdomen, legs, or feet.
Splinter hemorrhage and endocarditis. Splinter hemorrhages are bleeding areas that appear as splinter-like streaks under a nail bed — usually your fingernails. At first, they are red or purple but will turn brown or black in a matter of days. They happen when blood clots from a site of infection travel to other parts of the body and block the blood supply there. Splinter hemorrhages develop in up to a third of people with endocarditis. If you have endocarditis, splinter hemorrhages can indicate severe illness, and you should seek medical help right away.
Endocarditis Causes
Endocarditis is caused by germs that travel to your heart through your bloodstream. The bacteria enter your body through your mouth, skin, throat, or intestines and, under certain conditions, endocarditis develops. If you have a healthy heart, it's unlikely that you'll develop endocarditis. Your immune system typically eliminates harmful bacteria before it gets to your heart, and healthy heart valves are usually bacteria resistant.
Endocarditis risk factors
You're more likely to get endocarditis if you have heart problems or artificial heart valves because this is where infection-causing germs are likely to attach and multiply. Other risk factors include:
- A history of endocarditis
- Previous heart valve surgery
- Being older — endocarditis is more common in people older than 60 years
- Certain types of congenital heart conditions
- Heart valves that are damaged from infection and diseases such as rheumatic fever
- Implanted heart devices such as a pacemaker
- Having HIV
- Mitral valve prolapse with a leaking valve
- Dirty needles with illicit IV drug use
- Dental procedures or poor dental hygiene, which can promote bacterial growth inside your mouth
- An indwelling catheter used for certain medical procedures and placed inside your body for an extended time
Endocarditis Diagnosis
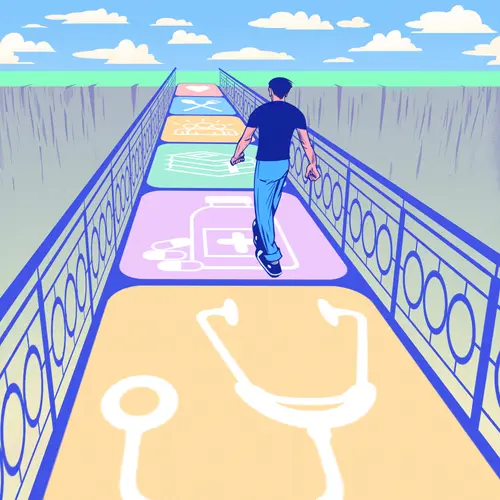
If you notice symptoms of endocarditis or your doctor thinks you might have it, they may suggest some tests. They'll also likely listen to your heart with a stethoscope to see if you have a new or changed heart murmur. If they need more information before making a diagnosis, they may order one or more of the following tests:
- Blood tests. These will look for bacteria in your bloodstream or show other things related to endocarditis, such as anemia, which means you don't have enough red blood cells.
- An echocardiogram or an EKG. This test shows how your heart is working. An echocardiogram uses an ultrasound device to produce images of your heart. An EKG uses sensors to measure the timing and length of your heartbeat.
- An X-ray. This will show if endocarditis has affected your heart or lungs.
- A CT scan or an MRI. This test uses pictures to show your doctor if the infection has spread to another area of your body like your brain or chest.
Endocarditis Treatment
In most cases, your doctor will prescribe antibiotics. Usually, you will stay in the hospital for about a week to receive them through an IV. You may need IV antibiotics for two to six weeks, but some of that might be from home.
Your team at the hospital will help you make arrangements to finish the medication and receive follow-up care.
In some cases, endocarditis requires surgery to completely clear it or to replace a damaged heart valve. Whether you need surgery will depend on your specific case and the type of infection you have.
Endocarditis Prevention
Understanding how to recognize the signs of endocarditis can help you get quick treatment. If you notice any symptoms, contact your doctor immediately. If you're diagnosed with endocarditis, you may want to get a special card from the American Heart Association to keep in your wallet.
Dental hygiene is an important part of endocarditis prevention. Germs from infections in your mouth can travel to your heart through your bloodstream and cause the infection. Always make sure to brush and floss your teeth and gums and go to the dentist regularly.
You should also be cautious about getting piercings or tattoos if you're at a higher risk of endocarditis. These kinds of procedures can make it easier for germs to get into your system. If you get a skin infection or cut that doesn't heal properly, you should contact your doctor.
Before getting any kind of medical or dental procedure, be sure to let your doctor or dentist know that you may be at a risk of endocarditis. That way, they can decide whether to prescribe antibiotics before your procedure as a precaution to keep you safe from infection.
Life Expectancy After Endocarditis
With early diagnosis and treatment, more than 90% of people with bacterial endocarditis recover. Those with a fungal endocarditis infection usually fare worse. Which side of your heart is affected can also alter your outlook. Those with right side endocarditis tend to do better than those with left side illness. If you've had a heart valve replacement, you are at the greatest risk of endocarditis in the year after your surgery, although the condition can develop at any time.
Endocarditis complications can include congestive heart failure, pulmonary embolism, stroke, heart attack, and kidney issues.
Without treatment, endocarditis can critically damage your heart or even be fatal.
Takeaways
Endocarditis is inflammation and infection of the heart's valves and inner lining, the endocardium. It's caused by bacteria, fungi, or other germs that travel through the bloodstream into the heart. People with an otherwise healthy heart are usually not at a risk of endocarditis, but you are more at risk if you have an implanted cardiac device, heart valves damaged by a congenital condition or disease, or a history of illicit IV drug use.
Endocarditis FAQs
Is endocarditis treatable?
It takes about two to six weeks to treat endocarditis with antibiotic therapy, usually begun in a hospital. The type of antibiotics used and the length of treatment depend on what organism has caused your infection. Sometimes, surgery is needed to replace a damaged valve.
Can you fully recover from endocarditis?
Early and aggressive treatment can help most people recover from endocarditis. However complete recovery depends on:
- How old you are
- Whether you have an artificial heart valve
- How long your heart has been infected
- What type of organism caused the infection
- The amount of damage to your heart valve
What are the warning signs of endocarditis?
Signs of endocarditis may develop slowly or all of a sudden. They include:
- Fever, chills, and sweating that last a long time or come and go and may be more pronounced at night
- Shortness of breath
- Swelling in the legs, feet, or abdomen
- Tiredness and weakness
- Appetite loss and weight loss
- Achy muscles or joints
- Bleeding under the nails (splinter hemorrhages)
- Painless red areas on your palms or the bottom of your feet
- Painful red lumps on the pads of your fingers or toes