Advances in Uterine Fibroid Treatment


Uterine Fibroid Treatment: Know Your Choices
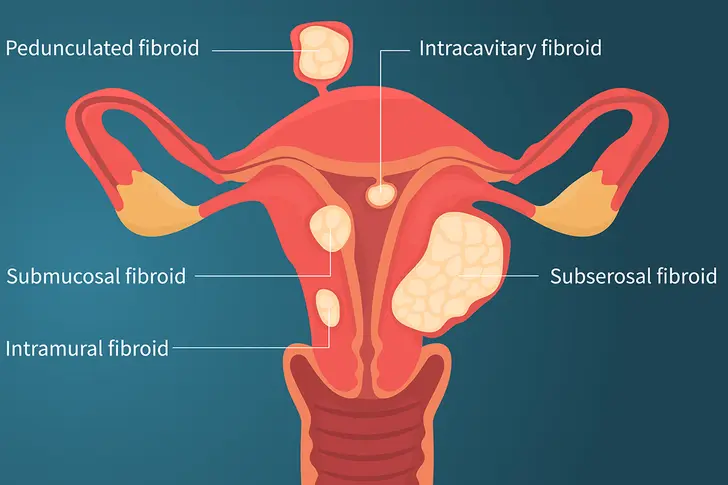
Uterine fibroids are noncancerous tumors that grow in the uterus. They’re really common in women and people who have a menstrual cycle, especially Black women. Fibroids don't always cause problems, but they can trigger symptoms like pelvic pain and heavy bleeding. Treatment includes medical therapy, hysterectomy (taking the uterus out), and a number of techniques in between. Ask your doctor for the full menu of treatment options.

Progestin-Only Intrauterine Device (IUD)
If your fibroids don’t affect the inside of your uterus, the doctor might want you to try a progestin-releasing intrauterine device (IUD). That’s a type of birth control that lasts for up to 5 years. Progestin-only IUDs don’t help you feel better by getting rid of fibroids. Instead, they may lighten or stop your period. This might ease symptoms caused by fibroids, including pain and heavy bleeding.

Gonadotropin-Releasing Hormone (GnRH) Agonists
These drugs block the hormone that triggers your menstrual cycle. As a result, your period stops and fibroids shrink. This is a short-term treatment (6 months or less) sometimes used before surgery because smaller fibroids are easier to remove. GnRH agonists also block sex hormones like estrogen. This can cause unwanted side effects. You may get menopause-like symptoms like bone loss, vaginal dryness, and hot flashes.
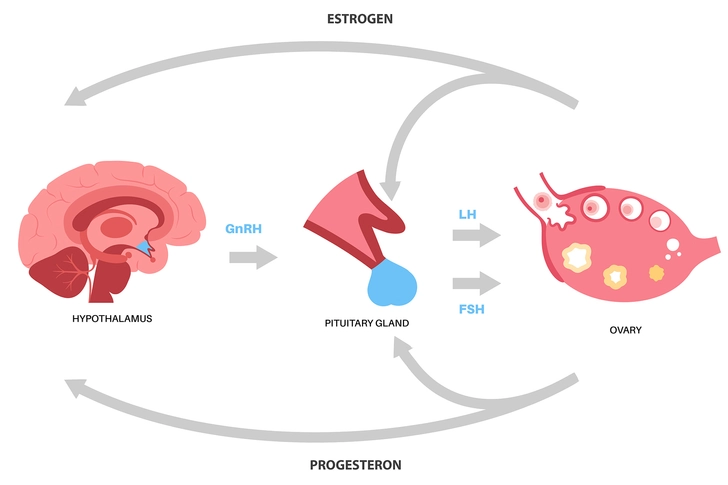
Other Hormone Therapies
Uterine fibroid treatment without surgery may include GnRH antagonists. These drugs don’t shrink fibroids, but they may treat abnormal bleeding for up to 2 years. You may need to take other lab-made hormones at the same time to lessen side effects like hot flashes and bone loss. This is called add-back therapy. Scientists continue to study other ways to manage fibroid symptoms, such as selective progesterone receptor modulators (SPRMs). These drugs may ease heavy bleeding as well as others. But we need more research to know for sure.
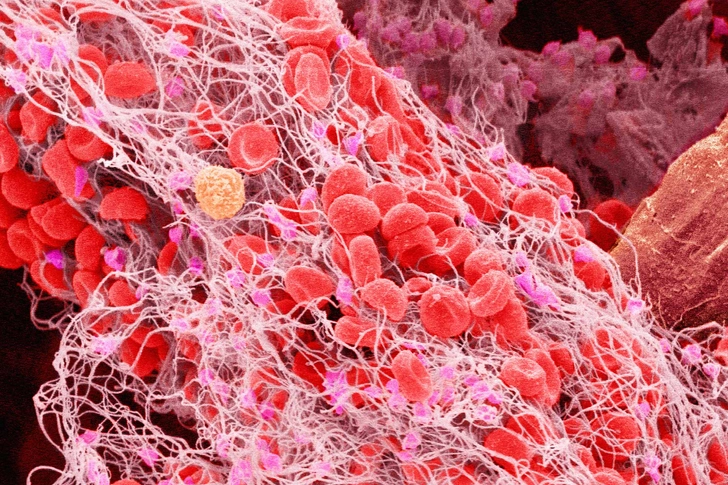
Tranexamic Acid
You won’t take this drug to stop your menstrual cycle. And it won’t shrink your fibroids. But it can block the breakdown of blood clots and lessen heavy bleeding. It’s important to ask your doctor when and how often you should take tranexamic acid. But it’s typically something you’ll use only during your period.

MRI-Guided Focused Ultrasound (FUS)
This newer technique targets fibroids from the outside. Your doctor will put you inside an MRI machine to pinpoint the tumors. Then they’ll use sound waves to heat and break down the tissue. This may take a few hours. You should feel back to normal within a few days. But it may take 3-6 months for your fibroids to get smaller. MRI-guided FUS isn’t right for everyone. It shouldn't be used during pregnancy.
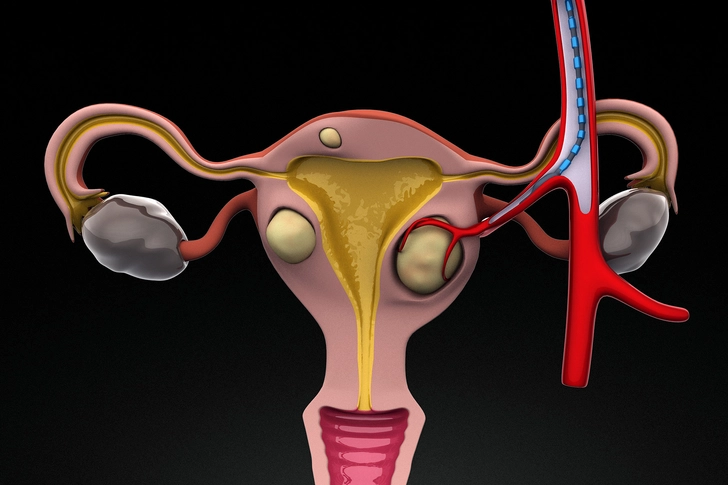
Uterine Artery Embolization (UAE)
Your doctor will make a small poke in your skin. They’ll use a thin tube to put tiny bits of plastic or gel into the blood vessels that go to your uterus. This cuts off blood flow to the fibroids and shrinks them. You may have less pain, pressure, or bleeding after UAE. But you might have trouble getting pregnant later on. And your fibroids may grow back. Around 1 in 5 people needs another fibroid surgery down the road.
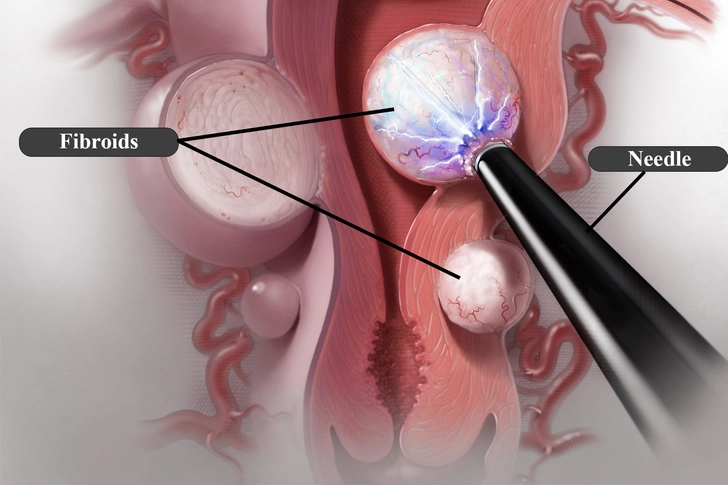
Radiofrequency Ablation (RFA)
RFA uses small needles to heat and destroy fibroids and their blood vessels. The tissue may continue to die for up to a year after surgery. RFA is commonly done one of two ways. You may get a laparoscopy (Acessa). That’s when your doctor makes two small cuts in your belly and uses a special camera to find the fibroids. Another way is to go through your vagina and cervix (Sonata). RFA is generally considered safe. But we need more research to know if it’ll hurt your chances of getting pregnant later.
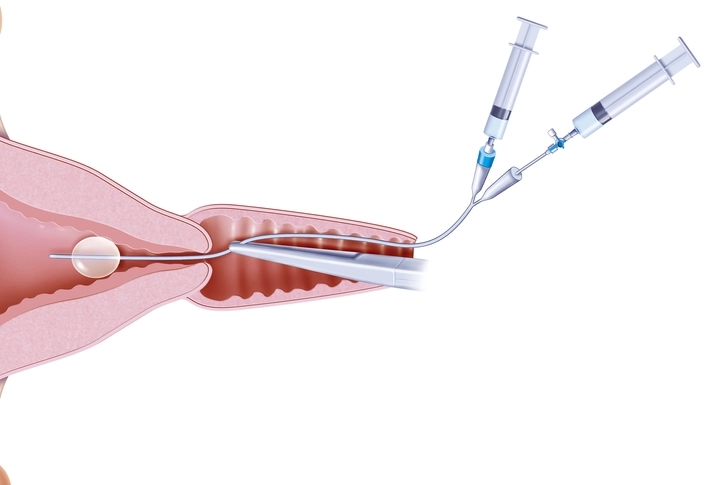
Endometrial Ablation
This treatment might be used to control heavy bleeding when medication isn't enough. The doctor won’t make any cuts in your belly. Instead, they'll get to your uterus through your vagina. The procedure thins the lining of your uterus with things like electricity, heat, or cold. You’ll go home the same day and should recover within a day or two. You may not be able to get pregnant or safely carry a baby after endometrial ablation.
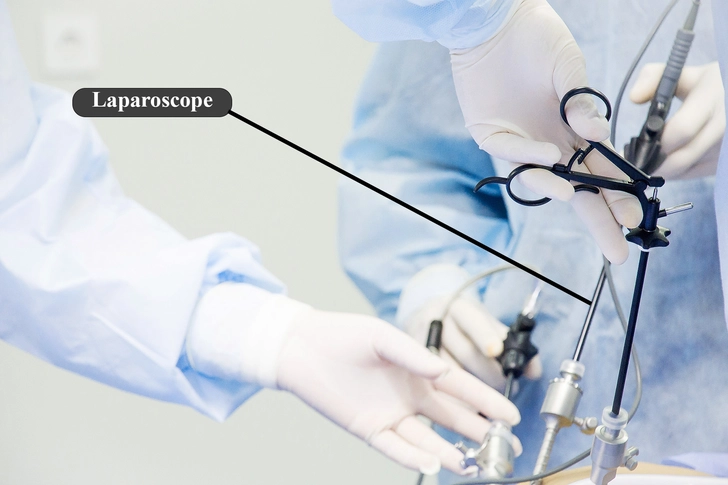
Laparoscopic or Robotic Myomectomy
A myomectomy removes fibroids but leaves your uterus. If you don’t have very many, your doctor may only need to make small cuts in your belly (laparoscopy). Then they’ll use a special camera (laparoscope) to see inside your body. Once they find the fibroids, they’ll use small tools to cut them out. A robotic myomectomy is a type of laparoscopy. But your surgeon uses a special machine to get a zoomed-in view of your uterus.
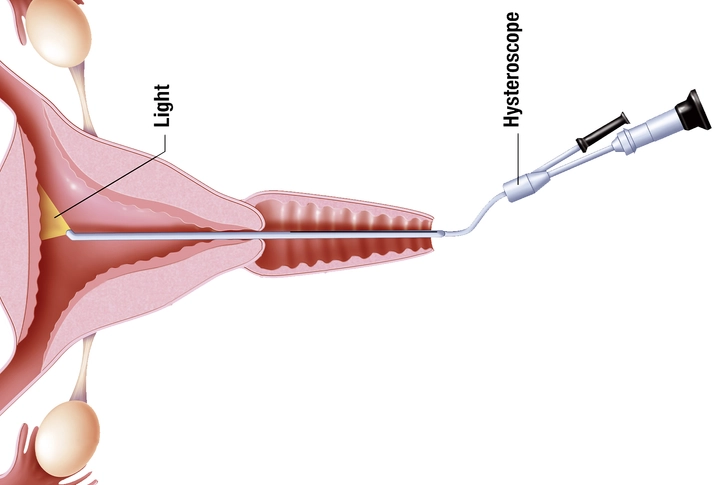
Hysteroscopic Myomectomy
This is another way to treat fibroids without making cuts in your belly. Your doctor can put a thin, hollow tube (hysteroscope) through your vagina into your uterus. Other tools slide through this tube. One is called a resectoscope. It can destroy fibroids by blasting them with laser beams. A hysteroscopy can shrink fibroids inside your uterus, but it can’t treat the ones deep in the uterine walls.

Abdominal Myomectomy
This option also lets you keep your uterus. But your doctor will need to remove fibroids through a big cut in your belly. This kind of surgery is more likely if your fibroids are really big, hard to get to, or you have lots of them. Go over the pros and cons of an abdominal myomectomy with your doctor. It may cause scarring that’ll hurt your chances of getting pregnant later.

Will You Need a Hysterectomy?
Most people with fibroids don’t need to remove their uterus. But a hysterectomy is sometimes the best choice if you have large fibroids or serious bleeding that’s hard to control with other treatments. And this procedure is the only surefire way to get rid of fibroids for good. While you won’t be able to get pregnant afterward, you may be able to keep your ovaries. Ask your doctor what’s right for you.

When to Get Treatment for Uterine Fibroids
Tell your doctor if you have heavy menstrual bleeding or vaginal bleeding outside of your period. Also tell them if you have pelvic pain that doesn’t go away, swelling or a feeling of fullness in your lower belly, the urge to pee a lot, or trouble pooping. Fibroids are usually harmless, but they can affect your health and quality of life. Your doctor can help you figure out what kind of treatment, if any, is best for you.

Can You Prevent Fibroids?
Scientists don’t know how to stop fibroids from forming. There’s ongoing research in this area. But certain healthy lifestyle choices may lower your odds of getting them. That includes eating less red meat and more fruits and vegetables. Ask your doctor to check how much vitamin D you have in your blood. People who don’t have enough of this key nutrient seem to have a greater chance of fibroids.
IMAGES PROVIDED BY:
- Viktoriia Ilina / Getty Images
- Mariakray / Getty Images
- yacobchuk / Getty Images
- Pikovit44 / Getty Images
- Micro Discovery / Getty Images
- skynesher / Getty Images
- Jos?? Antonio Pe??as / Science Source
- DNA Illustrations / Science Source
- BSIP / JACOPIN / Medical Images
- smirart / Getty Images
- BSIP / JACOPIN / Medical Images
- nortonrsx / Getty Images
- Shannon Fagan / Getty Images
- Burak Karademir / Getty Images
- Arx0nt / Getty Images
SOURCES:
Linda Fan, MD, FACOG, assistant professor of obstetrics, gynecology, and reproductive sciences, Yale School of Medicine.
American College of Obstetricians and Gynecologists: “Uterine Fibroids,” “Uterine Artery Embolization (UAE),” “Endometrial Ablation.”
Cochrane Database of Systematic Reviews (CDSR): “Selective progesterone receptor modulators (SPRMs) for uterine fibroids.”
Stanford Medicine: “MrgFUS to Treat Uterine Fibroids.”
Yale Medicine: “Uterine Myoma (Fibroids).”
Office on Women’s Health: “Uterine fibroids.”
Mayo Clinic: “Uterine fibroids.”