Richard Core is a retired journalist living in Los Angeles who has had multiple sclerosis since 2004. After the disease’s initial attack, he continued working 15 years as a news editor and manager. He has been on more than a half dozen different disease-modifying therapies and has lived through multiple MS flare-ups. He credits regular exercise, a healthier diet and reduced stress with keeping his symptoms mostly stable for the last several years.
Soon after my neurologist broke the news that I had multiple sclerosis, he handed me a prescription for an antidepressant. “Uh, I’m not depressed,” I told him. “You will be,” he replied. His bedside manner notwithstanding, he knew the odds. At least half of all people with MS experience depression at one time or another, according to research studies. I took his advice and started taking the pills.
In my case, the doctor’s news was actually a momentary relief, finally confirming what I had strongly suspected. At that point, I had been living with MS for almost a year without a diagnosis. Due to my health insurance, I had been tied to a medical facility that didn't have an MS specialist in its neurology department.
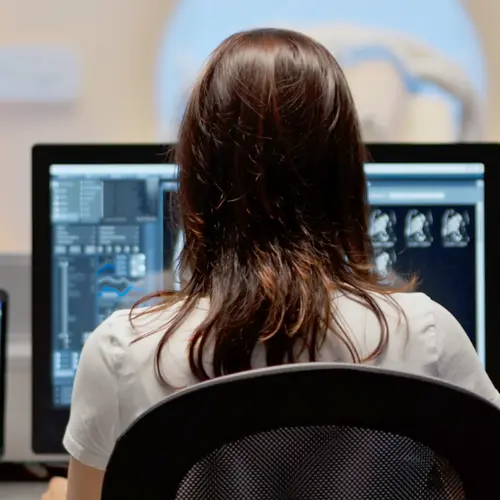
I had been assigned an epilepsy specialist who apparently didn’t know — nor did I at the time — that an MRI exam would have shown the lesions in my brain and spine, confirming I had MS. He put me through a few spinal taps, which were inconclusive, but never ordered an MRI.
For nine months I kept telling him I had MS, only to have him respond: “We don’t know that.” I based my argument on my mom’s stories of how her mother, who died before I was born, had likely had the disease, although it was not diagnosed then. I also did my research online. My grandmother’s symptoms and those described on various websites closely matched mine. During those nine undiagnosed months, I experienced two more attacks that left me with even more weakness, numbness and tingling in my legs and feet.
Was I depressed during this time? It’s hard to say. I just remember being determined to keep pushing, to not give in to whatever was going on in my body. I wouldn’t allow myself to let up at work or in other commitments. My parents instilled that attitude in me. I learned from them that when times are tough or I’m feeling down, I should try to find work or other things to keep me occupied. I can sort through my problems better while being productive, rather than sitting on the couch or lying in bed. I’ll leave it to others to determine whether that perspective is a good approach for mental health.
Still without a diagnosis, I continued to work my high-stress, long-hours job as the editor of The Los Angeles Times website. I limped badly around the office, but all I could tell co-workers was that my doctors didn’t know what was wrong. My lack of an explanation led to lots of suspicious looks and whispers that I had suffered a nervous breakdown. Outside of work, I continued to referee my 10-year-old daughter’s Saturday soccer matches, dragging my gimpy right leg up and down the field.
When I finally got my MS diagnosis, it came as a relief: my self-diagnosis was confirmed, and I knew what was wrong.
About a year after getting the diagnosis and the Wellbutrin prescription, I stopped taking the antidepressant, which didn’t seem to be doing much. At the same time I started seeing a psychologist on the staff at my MS clinic. I still check in with her periodically.
I became an inaugural member of a monthly MS support group at my clinic, and then also joined an offshoot men’s support group. I still participate in both, more than 15 years later.
These individual and group sessions allow me to vent my frustrations, share happy moments, hear about others’ challenges, and break any feelings of isolation I may be slipping into. Exercise, projects around my home and volunteer work also give me outlets that clear my mind and lift my spirits.
Talk to your doctor about what might be helpful for your mental health. Your doctor can tell you about your options and help you weigh their pros and cons.